Osteoporosis
Osteoporosis is an increasing health problem worldwide. It affects more than five million people in Italy and it is the underlying cause of bone fractures occurring after age 50. The WHO (World Health Organization) ranks osteoporosis among the most pressing health problems of the last 10 years.
Osteoporosis is a condition of reduced bone mass and disruption of bone microarchitecture, thus leading to skeletal frailty and consequent increase of fracture risk even after simple daily activities, such as raising from sitting, walking, or lifting small weights.
Fractures of the spine and hip seriously compromise range of motion and limit independent living. Unfortunately, osteoporosis frequently goes undiagnosed until a fracture occurs. FIROMMS is wholly devoted to promote prevention, diagnosis and treatment of such a disabling condition.
Bone life
The decalcification of bone tissue, is the base of osteoporosis, this is determined by an imbalance in the physiological processes which regulate bone life.
In fact, bone development does not stop with adolescence, but continues for all our life: in fact our bones are constantly formed and damaged in small parts, remodelling, so they can adjust themselves to the variation in body weight and body movement.
This ongoing transformation in the form and consistence of the bone is regulated by the activity of two types of cells. The osteoclasti and the osteoblasti, which are present in the bone tissue, and which work in a coordinated manner.
The osteoclasti destroy old bone tissue and make way for new tissue which is produced the osteoblasti: However, when the osteoclasti destroy more tissue than what the osteoblasti can reproduce, the bone loses consistency, and thus develops osteoporosis.
This process of destruction and construction of the bone is mainly governed by two hormones:
1) paratiroideo hormone, or paratormone, favours the action of osteoclasti and therefore the demolition of old bone;
2) calcitonina, which inhibits the destructive cells and supports the reconstructive activity carried out by the osteoblasti.
However, many other factors intervene to regulate the correct function of the bone cells.
An important role is played by the sex hormones, (testosterone e estrogeni) and some nutrients like calcium and vitamin D
The bone metabolism undergoes changes with time.
In the first phase of life, the production of bone tissue is very intense and leads to the *’peak’ of bone mass between the ages of 18 and 25 (* the highest level of bone density that an individual will reach)
In the second phase, which lasts for some years, the bone mass remains almost unchanged, as the remodelling process carried out by the bone tissue cells remains constant.
In the third phase, around the age of thirty, there is a slow and gradual diminution in the production of new bone and therefore a reduction in the values of bone mass.
Correct lifestyle can prevent osteoporosis
It is also fundamental to assume a correct diet.
The skeleton must take in the right amount of calcium in order to grow and be strong and healthy.
Calcium is the main mineral in our organism and is needed in order to make our bones strong: however, as the human body cannot produce calcium on its own accord, we need to take it in it through our food and drink.
A diet rich in milk and dairy products is fundamental to guarantee our organism the correct amount of calcium: Calcium is taken out of our food through the digestive process and then passed on through our blood, where the concentration of calcium is kept under control.
If the level of calcium is too high, it is eliminated through our urine or deposited in our bones; if the level of calcium is too low ( e. g as a result of poor intestinal absorption or too low an intake), the organism will then take the calcium from the main reserve area: the skeleton
The absorption process of calcium is regulated by our hormones and influenced by our alimentation: the excessive assumption of vegetable fibre, caffeine and cigarette smoke, excessive alcohol, animal protein and sodium are all extremely harmful to bone cells.
Vitamin D is also essential, our organism must have a substantial supply.
Vitamin D favours an improved absorption of calcium and phosphor within the intestines, it also helps maintain the correct levels of calcium in our blood and helps to guarantee a sufficient mineralization of the skeleton.
The presence of this vitamin is determined by the exposure to sunshine , thanks to the action of ultra violet rays ( UV), which stimulate the synthesis on the inside of the skin: it is sufficient to expose yourself to sunshine for 10 to 15 minutes a day, even if it is only those areas which are normally exposed ( face ,hands, arms).
Alternatively, vitamin D must be taken in, with food or by taking food supplements.

Diagnosis and treatment
The test used to identify the presence of osteoporosis and to follow the evolution of the disease is the bone densitometria or MOC ( the mineralometria ossea computerizzato) The techniques to measure the level of the various skeletal segments are diverse. Today, the technique which is considered to be the most accurate and sensitive, is the duel energy X- ray absorptiometry (DEXA or DXA) which uses minimal doses of x- rays.
The test is non invasive, does not require any patient preparation and lasts between 5 and 10 minutes: because of this, this test for bone mineral density, should be a routine test, which should not only be carried out on those who are considered to be at risk (men and women with one or more factors), but also men and women much younger.
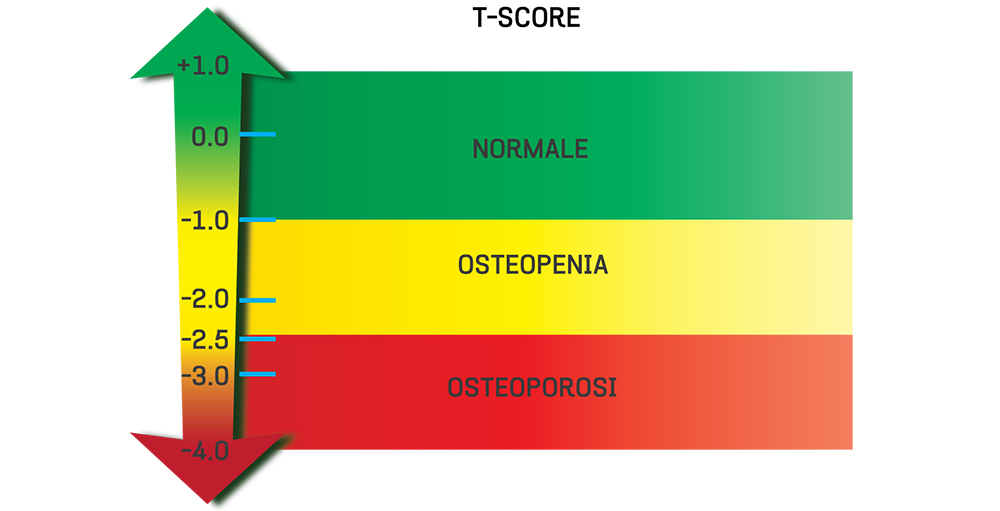
The T-Score
The measurement of mineral bone density is both a reliable and safe method to evaluate the risk of fracture occurring, within the next five years: It is usually advised to undergo the bone mineral density test at the age of 65. Although there are risk indicators, which would indicate that the exam should be done before the age of 65, not only for women who have already gone through the menopause but also for men: in fact , once over the age of fifty, with every ten years, the risk doubles or triples when there is a sudden reduction in body weight (e. g weighing less than 57 kg),height, falls, a family history of fractures, inflammatory disturbances which affect the gastro-intestinal system, muscular skeletal pulmonary systems, a delay in the first menstruation( after the age of 15), the assumption of cortisonici or discontinued hormone replacement therapy in post menopause.
Once osteoporosis is diagnosed, the test needs to be repeated every 2 years, every 5 years if the parameters result as being within the norm.
MAIN FRACTURE SITES
Often, we only discover the presence of osteoporosis when a fracture happens without there actually having been a significant incident e. g a fall.
The reason for not identifying osteoporosis earlier, is due to the fact that the reduction of the bone mass goes on for years, without showing any signs at all.
The disease is even more difficult to diagnose because early fractures related to the weakening of bones, show signs which are often confused with other pathologies:
e. g the first area affected by osteoporosis is usually the vertebrae, showing symptoms which include pain in the dorsal and Lombard region, an imperceptible reduction in height, gradual alterations to the curve of the spine, all of which are very rarely taken into consideration .
For this reason, the number of people who are diagnosed as having osteoporosis are less than those who are actually affected. In order to reduce this gap, FIROMMS has set up the P.R.O.S.I.T project, which is carrying out a large scale study on the elderly population in Italy.
After osteoporosis has been diagnosed, to improve the individual’s well being, a better lifestyle should be integrated with a suitable drug therapy
There are two main aims: to slow down as much as possible the loss of bone mass and reduce the risk of fractures.
The treatments available fall into two main categories: drugs which block the bone re absorption, which is caused by the osteoclasti and drugs which stimulate the production of new bone tissue on behalf of the osteoblasti.
The so called anti-absorption drugs belong in the first group:
Bifosfonati
SERM or selective modulatori of receptors for estrogens.
Hormone replacement therapy for women in menopause
Calcitonina
In the second group of drugs, there is a synthetic form of paratormone, the paratiroideo hormone which favours the absorption of calcium in tubuli distali , which inhibits the re absorption of phosphate and stimulates l’idrossilazione of vitamin D and strontium ranelate.
Strontium ranelate, a parent of a new class of drugs dual action, stimulating bone formation through the Ca-sensitive receptor present on osteoblasts and inhibiting bone resorption through the system OPG / RANK / RANK-L. Strontium ranelate has been shown to reduce the risk of vertebral and hip fractures in patients with postmenopausal osteoporosis.
It is also the first and only drug available to date with evidence of protection from the risk of fracture in the long term both vertebral level femoral.
When deciding which treatment to use, the specialist will evaluate the advantages and disadvantages ( side effects) of each therapy, especially when considering using hormone replacement therapy for menopausal women.
The research into new drugs has recently produced a new one which belongs to the family of bifosfonati, more commonly known as zoledronic acid. This drug has a big advantage because it only needs to be given once a year, via intravenous injection.
A potential, natural alternative (represented by fitoestrogeni ) to hormone replacement therapy is arousing a lot of interest.
Fitoestogeni is a molecule that is found in many plant species, both for alimentary and medicinal use, it imitates or modulate the action of estrogens.
We need to combine the taking of calcium and vitamin D supplements, together with the chosen drug therapy, because with the aging process there is a diminution of the ability to absorb calcium through the intestines and a reduction in the endogenous production of vitamin D.
Different type of osteoporosis
The osteoporotic process is totally normal: Senile osteoporosis is where the bone tissue undergoes a natural and progressive rarefaction, which can also be seen in healthy individuals of both sexes, around the age of seventy. In this case we are talking about type 2,
However, women are affected by a more precocious and serious form of osteoporosis, type 1, which is closely connected to the menopause and to the sudden decline in estrogen which is associated with the disappearance of the menstrual cycle.
There are also other forms of secondary osteoporosis which are caused by certain illnesses or by the negative effects that certain drugs can have on the individual.
When any individual has any of the following problems they are more likely to get osteoporosis i.e.
Those who have endocrine disturbances which affect the sex hormones, the thyroid or surrenalici.
Metabolic imbalance
Chronic disease of the muscular skeletal system
Inflammation of the intestine
Any condition which leads to prolonged immobility
Osteoporosis is a disease influenced by various factors: genetic, environmental, nutritional, metabolic and/or connected to lifestyle. In order to identify these factors with precision and understand their effects, FIROMMS has set up the P.RO.S.I. T project.
When there is a re-occurrence of the disease in the same family, we begin to suspect a hereditary predisposition.
However, scientists are still not sure just how much genetics can determine the presence of the disease, even if it is presumed that certain genes are involved in regulating both the development of bone mass, in infancy and in adolescence, and the speed in which this bone mass reduces in old age.
There are a number of important constitutional elements documented.
For example, those individuals who have a small frame, little muscle and are extremely thin, are at more risk than those that who are tall with a higher body mass.
For women, the length of their fertile period is extremely relevant, because this determines the length of time that their body is exposed to the estrogens hormone:
The later the oncoming of the first menstruation in puberty and the sooner the arrival of the climaterio in adulthood, the greater the risk of osteoporosis in post menopausal women.
RISK FACTOR
– The diagnosis of osteoporosis or fractures caused by slight traumas, in people from the same family.
– Old fractures as a result of a slight trauma
– Noting a recent diminution in stature or an alteration in the spinal curve
– The presence of predisponenti illnesses: hormonal imbalance (ipogonadismo, iperparatiroidismo, cushing syndrome, chronic illness) liver failure, broncopneumopatia chronica ostruttiva- BCO, heart failure, rheumatoid arthritis, spondilite anchilosante, crohns disease, celiachia or tumours (multiple melanoma)
– The prolonged intake (for longer than 3 months) of drugs that provoke osteoporosis ( cortisonici, immunosoppressori, anti-tumours, thyroid hormones, anti- convulsivanti, anti-depressants, anti- acids and diuretics)
– A long period of immobility, caused by being bed-ridden, accidents or having had surgery
– Being excessively thin or obese
– A diet lacking in calcium and vitamin D
– A sedentary lifestyle
– Heavy smoking
– Alcohol abuse
Regarding women only:
– The late arrival of the first menstruation (later than 13)
– Long periods without menstruation (amenorrhea) before the menopause
– Precocious menopause ( before the age of 45)
It is also fundamental to learn to assume a correct posture which will prevent putting stress onto our spine.
